Abstract
Introduction. Minimal residual disease (MRD) detection by multicolor flow cytometry (MFC) after early induction or consolidation AML therapy is a well known factor of adverse prognosis, especially in intermediate risk group. New assessment of response in AML is complete remission with MRD-negative status. However, there is still no standardization of MFC method for AML patients (pts). Optimal time point for MRD status and its threshold value vary in different studies.
Aim. To study different consolidation treatment regimens in AML pts by measuring of MRD reduction, to determine optimal time point and threshold level for additional risk stratification.
Patients and methods. From March 2016 to February 2018 42 pts (younger than 60 y.o.) with newly diagnosed AML were included in prospective MRD study in hematology department of National Research Center for hematology. Initial leukemia-associated immunophenotype was analysed before any treatment, and bone marrow assessment for MRD detection was performed in CR pts after 1st and 2nd chemotherapy courses. The standard antibody panel included CD19, CD7, CD2, CD38, CD65, CD66b, CD99 (FITC); CD56, CD15, CD11b, CD13 (PE); CD33 (APC); HLA-DR, CD14, CD16, CD117 (PerCP-Cy 5.5); CD45 (APC-H7) and CD34(PE-Cy7). For results record BD FACSCanto II (Becton Dickinson) machine was used. The first course for all pts was the standard «7+3». Before March 2017 the second course was also «7+3» and included 25 pts, after March 2017 - 17 pts received intensive «Flarida» regimen (Fludarabine 30mg/m2 1-4, Ara-C 1g/m2 1-4, Idarubicin 8mg/m2 1,3). The 2nd MRD test was compared in these two groups. There was no difference between the two groups by pts in CR after the first «7+3», ELN status and age.
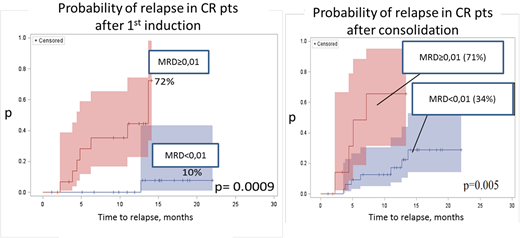
Results. By using of special mathematical and statistical method the threshold value of 0,01% was estimated for long-term prognosis. Two years relapse-free survival (RFS) in MRD-positive (MRD+) and MRD-negative (MRD-) groups after the 1st induction was 23% and 87%, respectively (p<0,01). Probability of relapse (PoR) during the first year of observation in these two groups was 72% and 10%, respectively (p<0,01). After the second course 9 more pts in two groups became MRD-negative and 6 of them developed a relapse. RFS in MRD+ and MRD- after the 2nd course was 36% and 65% (p<0,01), and PoR - 71% and 34%, respectively (p<0,01). Multivariate analysis showed MRD factor as the only important in RFS compared to cytogenetic, molecular status, age and initial leukocyte count. OS and RFS in «7+3» and «Flarida» regimens during the first year were 100% vs 80% (p=0,27) and 74% vs 76% (p=0,63), respectively. MRD level reduction after different consolidation regimens («7+3» vs «Flarida») didn't show any variation (p=0,14) and there was no association between MRD status after induction in different ELN groups (p=0,52).
Conclusion. MRD threshold value of 0,01% allows to distinguish the two cohorts of AML pts groups: with different prognosis even in any ELN risk subgroups. The RFS was reliably higher in pts with CR and MRD-negative status right after the first induction, which reflected the chemo sensitivity of the tumor. After the consolidation course MRD detection still has a prognostic value. MRD level reduction was not associated with intensification of chemotherapy. There is a great need to achieve MRD negative status in AML pts after the 1st induction course so new therapy approaches are pending.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal